COVID-19 Vaccine and Myocarditis
Risk of Myocarditis after COVID Vaccine
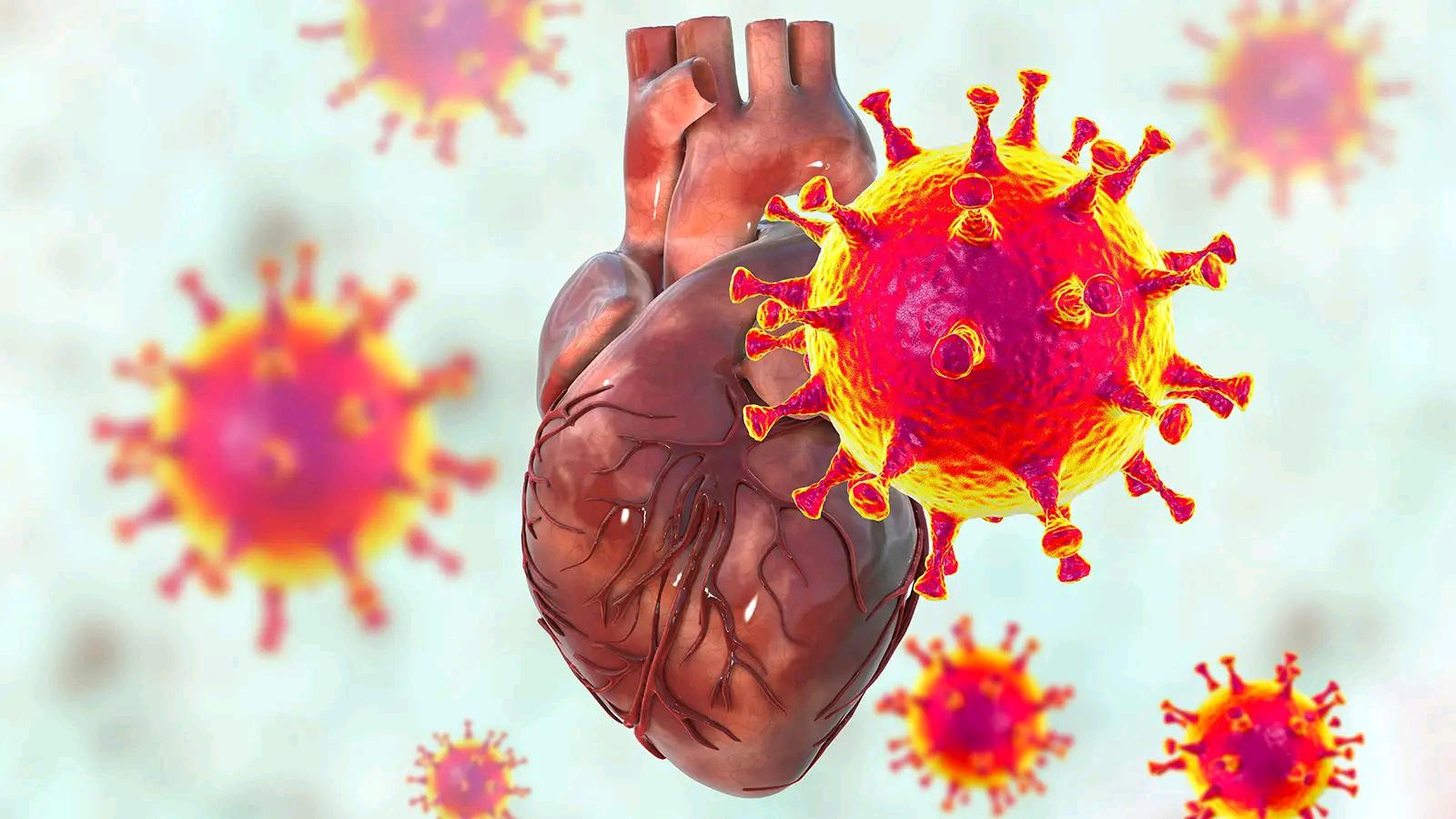
Researchers are working day-and-night to improve the vaccine to fight COVID-19. The U.S. COVID-19 vaccination rates move forward, but one of the side effects is gaining attention is a type of inflammation in the heart muscle called myocarditis.
Based on passive surveillance reporting in the US, the risk of myocarditis increases after receiving mRNA-based COVID-19 vaccines. The risk has been observed across multiple age and sex strata. As per the data the risk was highest after the second vaccination dose in adolescent males and young men. It is important to consider this risk in the context of the benefits of COVID-19 vaccination.
What is Myocarditis and how is it Caused?
Myocarditis is a disease affecting the heart muscle or myocardium. The heart muscle contracts and relaxes to pump blood in and out of your heart as well as to the rest of the body. The heart muscles become inflamed, reducing the ability to pump blood. This may lead to problems like an abnormal heartbeat, chest pain, and trouble breathing.
In extreme cases, it can lead to blood clots prompting a coronary failure or stroke, harm to the heart, or passing. Ordinarily, inflammation is your body's reaction to an injury or contamination. For instance, when you cut your finger, the tissue around the cut rapidly puffs up and becomes red. These are exemplary indications of inflammation, during which the phones of your safe framework race to the site to start fixes.
Myocarditis ordinarily results from viral contamination or a medication response. The most common viral infections include those that cause the common cold, influenza, or COVID-19. It can happen to anybody, including grown-ups, kids, and newborn children. It's bound to influence individuals under 30 who are generally solid. It influences men two times as frequently as ladies.
Autoimmune diseases like lupus, sarcoidosis can also cause myocarditis as the immune system can attack any organ in the body, including the heart, causing inflammation. Drugs or other natural or harmful openings can prompt myocarditis also.

How to Identify Myocarditis?
Myocarditis can range from mild to severe. It also affects children differently.
In mild cases, symptoms can include:
- Chest pain
- Shortness of breath
- Heart flutter
In severe cases, you might notice:
- Chest pain
- Rapid or abnormal heart rhythms
- Shortness of breath, at rest, or during physical activity
- Swelling in your legs, ankles, and feet
- Fatigue

Other symptoms can be part of a viral infection that causes your myocarditis, such as a headache, body aches, joint pain, fever, a sore throat, or diarrhea.
What leads to Heart Inflammation after COVID-19 Vaccine?
The experts aren’t sure of the link between COVID and Myocarditis. As per the data, only about 1,000 people have gotten vaccine-related myocarditis.
It has been observed that myocarditis seems to occur:
- In adolescent and young adult males 16 years or older
- After the second dose of one of the two mRNA COVID-19 vaccines
- Within several days after getting the vaccine
It is also observed that most people affected with myocarditis recovered quickly after getting treatment and some rest. The doctors are monitoring the side effects but need more research to know for sure what the causes and long-term effects might be.
Scientists say there might be a connection. One review tried more than 19,378 school competitors for COVID-19 contamination. Approximately 3,000 tried positive for COVID. Around 2,800 went through cardiovascular testing, and just 21 showed heart issues. Practically every one of the people who did recuperate completely. Specialists say there's little opportunity of myocarditis or other heart issues from COVID-19 contamination.
How Is It Diagnosed?
Early diagnosis is key for appropriate treatment, full recuperation, and forestall long-haul heart issues. Your primary care physician might do an actual test and get some information about your clinical history. They may likewise do lab and imaging tests to affirm how extreme the condition is. These can include:
- Electrocardiogram (EKG): This would help check your heart’s electrical signals and heart rate.
- Chest X-ray
- MRI
- Echocardiogram: This helps detect if your heart muscle has become inflamed and if it’s working properly.
- Blood tests
How is myocarditis treated?
The treatment of myocarditis relies upon the source and seriousness of the myocardial aggravation. Much of the time, myocarditis improves with appropriate measures, and you'll recuperate totally.
Some potential treatment options for myocarditis include:
- Corticosteroids: Corticosteroids help dampen or reduce the intensity of your immune response and help to lower inflammation levels.
- Cardiac medications: Myocarditis can have signs of heart failure and your doctor may prescribe a cardiac medication, such as Beta-blockers, ACE inhibitors, ARBs, and cardiac inotropes. This helps to reduce the amount of work your heart is doing.
- Diuretics: Therapy with diuretics can help reduce the accumulation of fluid.
- Ventricular assist devices (VAD): An extreme case of myocarditis, your heart needs help while it’s recovering. A VAD may be helpful to pump blood from the lower chambers of your heart to the rest of your body.
- Treating other conditions: Myocarditis caused due to a medical condition such as infection or an autoimmune disease, your doctor will also take steps to treat that as well.
These treatment options can assist with facilitating the heart's responsibility so it can mend itself. While you recuperate, your PCP may suggest:
- Getting plenty of rest
- Limiting your fluid intake
- Reducing the amount of salt in your diet
Assuming your myocarditis is serious and your heart is fizzling, other more obtrusive systems might be acted in the emergency clinic. Implantation of a pacemaker or a defibrillator might be vital. Whenever the heart is incredibly harmed, specialists might suggest a heart relocation.
What are the Complications of Myocarditis?
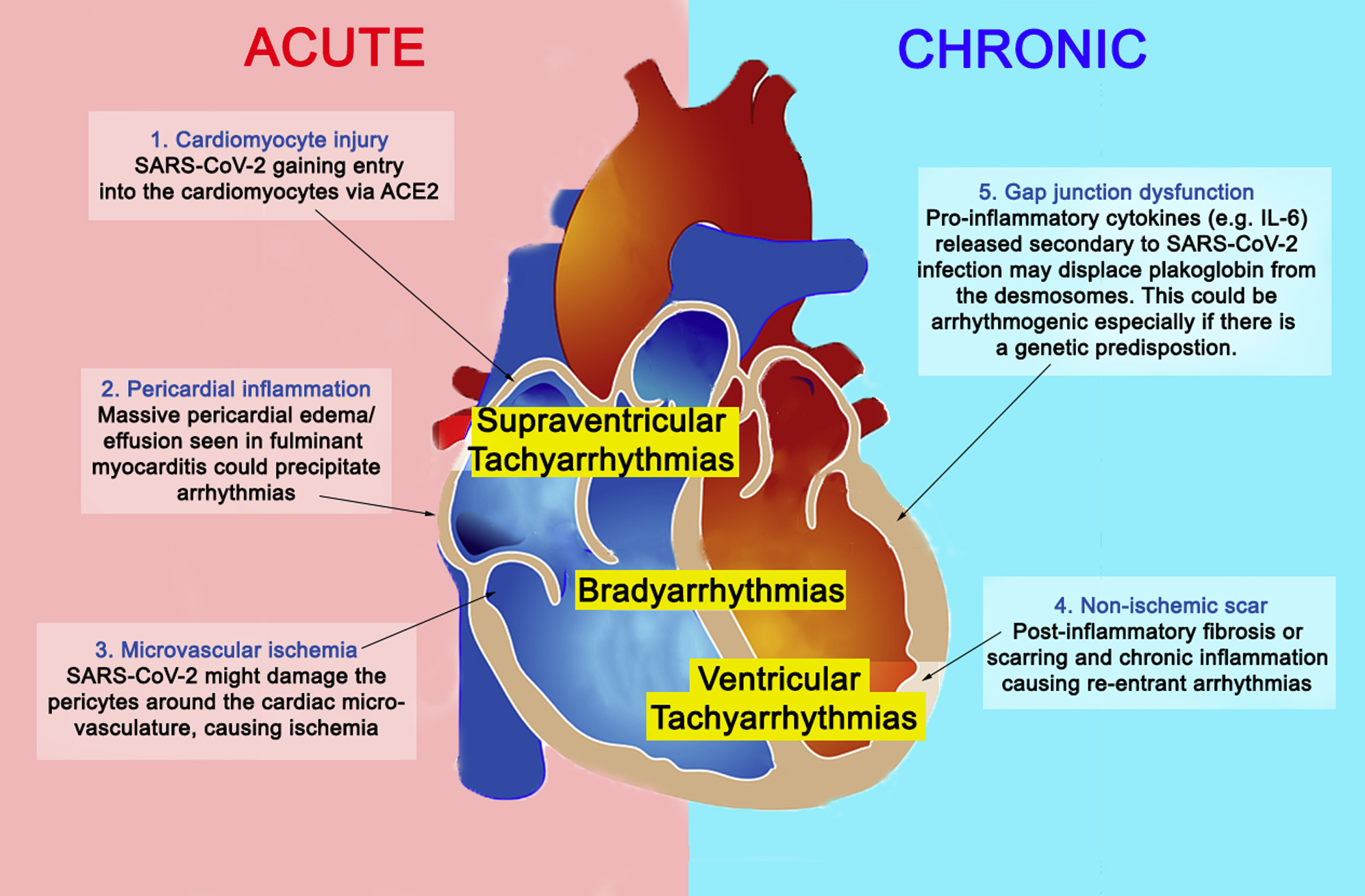
It's workable for myocarditis to make critical harm to the heart. Along these lines, an assortment of confusions can result, such as:
- Arrhythmia: Your heartbeat can be too fast, too slow, or irregular.
- Cardiomyopathy: Your heart muscle weakens and cannot pump blood effectively.
- Heart failure: Your heart has difficulty pumping enough blood to the organs and tissues of your body
- Heart attack: The blood supply to a part of your heart is cut off, causing heart tissue to die.
Outlook
After you get the COVID-19 antibody, keep an eye for side effects for as long as seven days after each dose. Tell your doctor quickly if you have sharp chest pain, a pounding heartbeat, or persistent heart flutters.
Assuming you notice myocarditis side effects or indications of an unfavorably susceptible response like hives, swelling, or wheezing after getting the antibody, let your PCP know about it or move clinical assistance immediately.
If you or anyone you know is suffering from the effects of Covid-19, our expert providers at Post Covid Centers will take care of your health and help you recover.
Call us on (469) 545-9983 to book a telehealth appointment for a home check-up.
People Also Read:
Post Covid Syndrome vs. Fatigue
While COVID-19 is a short-lived disease in most people, others experien...
Post Covid Syndrome vs. Skin Weakness Problems
A new study illustrates that some patients with COVID-19 disease have continuous skin-associated symptoms...
RELATED BLOGS