What is Mucormycosis?
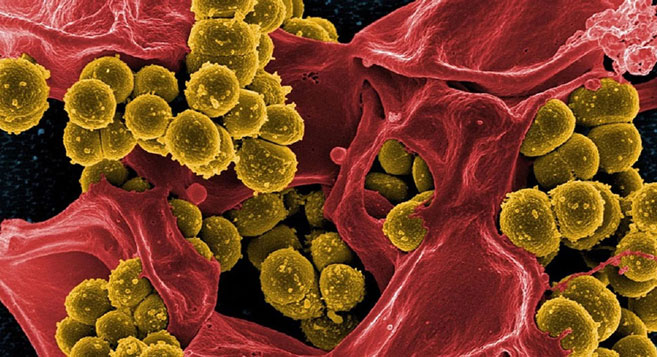
Mucormycosis (otherwise known as zygomycosis) is a severe yet rare fungal infection caused by a group of fungi known as mucormycetes. These fungi live throughout the environment, especially in soil and in decaying organic matter, for example, leaves, compost piles, or rotten wood.
People become infected with mucormycosis through contact with fungal spores in the environment. For instance, the lung or sinus forms of the infection could happen after someone breathes in spores.
These forms of mucormycosis generally happen in people who have health issues or take medicines that reduce the body’s capacity to fight germs and sickness. Mucormycosis could also develop on the skin after the fungus enters the skin through a cut, scrape, burn, or other forms of skin trauma.
Types of Mucormycosis
Rhinocerebral otherwise known as (sinus and brain) mucormycosis is an infection in the sinuses that could spread to the brain. This type of mucormycosis is most common in people with uncontrolled diabetes and in people who have had a kidney transplant.
Pulmonary mucormycosis (lung) is the most frequent form of mucormycosis in people in cancer patients and organ transplant patients or a stem cell transplant.
Gastrointestinal mucormycosis is more frequent among young children than adults, particularly premature and low birth weight infants less than one month of age, who have had antibiotics, surgery, or medicines that reduce the body’s capacity to fight germs and sickness.
Cutaneous mucormycosis (skin) happens after the fungi enter the body through a break in the skin (such as, after surgery, a burn, or another type of skin trauma). This is the most common type of mucormycosis among people who do not have weakened immune systems.
Disseminated mucormycosis happens when the infection spreads through the bloodstream to damage another part of the body. The infection most commonly damages the brain, but also could affect other organs for example the spleen, heart, and skin.
Types of Fungi that most frequently cause Mucormycosis
Instances are Rhizopus species, Mucor species, Rhizomucor species, Syncephalastrum species, Cunninghamella bertholletiae, Apophysomyces species, and Lichtheimia (initially Absidia) species.
Mucormycosis Symptoms
The symptoms of mucormycosis are dependent upon where in the body the fungus develops. Contact your healthcare professional if you have symptoms that you think are associated with mucormycosis.
-
Rhinocerebral (sinus and brain) mucormycosis Symptoms include:
- One-sided facial inflammation
- Headache
- Nasal or sinus congestion
- Black lesions on the nasal bridge or upper inside of the mouth that quickly become more serious
- Fever
-
Pulmonary (lung) mucormycosis Symptoms include:
- Fever
- Cough
- Chest pain
- Shortness of breath
Cutaneous (skin) mucormycosis could look like blisters or ulcers, and the infected region might turn black. Other symptoms include pain, warmth, excessive redness, or inflammation around a wound
-
Gastrointestinal mucormycosis Symptoms include:
- Abdominal pain
- Nausea and vomiting
- Gastrointestinal bleeding
Disseminated mucormycosis generally happens in people who are already sick from other medical conditions, so it could be difficult to know which symptoms are associated with mucormycosis. Patients with disseminated infection in the brain could develop developmental status changes or coma.
Mucormycosis Risk & Prevention
Who gets mucormycosis?
Mucormycosis is uncommon, but it is more frequent among people who have health issues or take medicines that reduce the body’s capacity to fight germs and illness. Specific groups of people are more likely to develop mucormycosis, including people with:
Diabetes, particularly with diabetic ketoacidosis
Cancer
Organ transplant
Stem cell transplant
Neutropenia (low number of white blood cells)
Prolonged corticosteroid use
Injection drug use
Excessive iron in the body (iron overload or hemochromatosis)
Skin injury because of surgery, burns, or wounds
Prematurity and low birthweight (for neonatal gastrointestinal mucormycosis)
How does someone get mucormycosis?
People become infected with mucormycosis through contact with fungal spores in the environment. For instance, the lung or sinus types of the infection could happen after someone inhales the spores from the air. A skin infection could happen after the fungus enters the skin through a scrape, burn, or other forms of skin injury.
Is mucormycosis contagious?
No. Mucormycosis is not capable of spreading between humans or between humans and animals.
How could I reduce the risk of mucormycosis?
It is hard to avoid breathing in fungal spores due to the fungi that cause mucormycosis are common in the environment. There is no vaccine to stop mucormycosis. For people who have weakened immune systems, there might be some ways to reduce the chances of developing mucormycosis.
-
Protect yourself from the environment – It is crucial to note that although these actions are suggested, they have not been proven to stop mucormycosis.
Try to circumvent regions with a lot of dust like construction or excavation sites. If you cannot avoid these regions, wear an N95 respirator (a type of face mask) while you are there.
Circumvent direct contact with water-damaged buildings and flood water after hurricanes and natural disasters.
-
Circumvent activities that involve close contact with soil or dust, for example, yard work or gardening. If this is not possible -
- Wear shoes, long pants, and a long-sleeved shirt when doing outdoor jobs for example gardening, yard work, or visiting wooded regions.
- Wear gloves when handling materials for example soil, moss, or manure.
- To lower the chances of developing a skin infection, wash skin injuries well with soap and water, particularly when they have been exposed to soil or dust.
Antifungal medication - If you are at high risk for developing mucormycosis (for instance, if you have had an organ transplant or a stem cell transplant), your healthcare professional might prescribe medication to stop mucormycosis and other mold infections. Doctors and scientists are still learning about which transplant patients are at the highest risk and how to best stop fungal infections.
Where Mucormycosis Comes From?
The fungi which cause mucormycosis lives in the environment
Mucormycetes, the group of fungi that cause mucormycosis, is present everywhere in the environment, especially in soil and in relation to decaying organic matter, for example, leaves, compost piles, and animal dung. They are more frequent in soil than in air, and in summer and fall than in winter or spring.
Most people come in contact with microscopic fungal spores every single day, so it is likely impossible to entirely avoid coming in contact with mucormycetes. These fungi are not harmful to the majority of people. Although, for people who have weakened immune systems, breathing in mucormycete spores could cause an infection in the lungs or sinuses which could spread to other parts of the body.
Types of fungi that lead to mucormycosis
Various different types of fungi could lead to mucormycosis. These fungi are known as mucormycetes and belong to the scientific order Mucorales. The most frequent types that lead to mucormycosis are Rhizopus species and Mucor species. Other instances include Rhizomucor species, Syncephalastrum species, Cunninghamella bertholletiae, Apophysomyces, Lichtheimia (formerly Absidia), Saksenaea, and Rhizomucor.

Mucormycosis Diagnosis
How is mucormycosis diagnosed?
Healthcare professionals consider your medical history, symptoms, physical exams, and laboratory tests when diagnosing mucormycosis. Healthcare professionals who suspect that you have mucormycosis in your lungs or sinuses may collect a sample of fluid from your respiratory system to send to a lab.
Your healthcare professional might perform a tissue biopsy, in which a small sample of affected tissue is analyzed in a lab for evidence of mucormycosis under a microscope or in a fungal culture. You might also require imaging tests for example a CT scan of your lungs, sinuses, or other parts of your body, depending on the location of the suspected infection.
Mucormycosis Treatment
How is mucormycosis treated?
Mucormycosis is a severe infection and requires to be treated with prescription antifungal medication, generally amphotericin B, posaconazole, or isavuconazole. These medications are given through a vein (intravenously IV) (amphotericin B, posaconazole, isavuconazole) or by mouth (posaconazole, isavuconazole).
Other medications, including fluconazole, voriconazole, and echinocandins, don’t work up against fungi that cause mucormycosis. Usually, mucormycosis needs surgery to cut away the contaminated tissue.
If you or anyone you know is suffering from mucormycosis, our expert providers at Post Covid Centers will take care of your health and help you recover.
Call 469-545-9983 to book a telehealth appointment for a home check-up.
Post Covid Syndrome vs. Fatigue
While COVID-19 is a short-lived disease in most people, others experien...
Post Covid Syndrome vs. Skin Weakness Problems
A new study illustrates that some patients with COVID-19 disease have continuous skin-associated symptoms...
RELATED BLOGS